Acute dystonic reactions are sudden, often distressing muscle contractions that can be frightening for patients and challenging for junior doctors. Understanding how to recognize and manage these reactions is crucial in the Emergency Department (ED). This guide will help you navigate history taking, examination, investigations, and management.
History Taking
When a patient presents with potential acute dystonia, it’s essential to gather a thorough history. Key questions to ask include:
Medication History:
Have you recently started any new medications? (Especially antipsychotics, antiemetics like metoclopramide, or antidepressants)
Have you missed any doses of your regular medications? Onset and Duration:
When did the symptoms start?
How quickly did the symptoms develop? Symptoms Description:
Can you describe the muscle contractions or spasms? (Which muscles are involved? Is there any pain associated?)
Have you experienced any similar symptoms in the past? Additional Symptoms:
Do you have any other symptoms, such as fever, altered mental status, or autonomic instability?
Have you had any recent infections or injuries? Personal and Family Medical History:
Do you have a history of neurological disorders or dystonia?
Is there any family history of similar symptoms?
Examination Findings
Perform a comprehensive physical examination with a focus on the following:
General Observation:
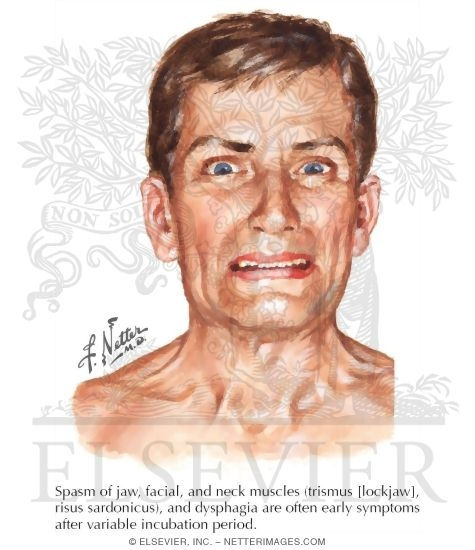
Note any obvious muscle contractions or abnormal postures.
Assess the patient’s level of distress and overall appearance. Neurological Examination:
Evaluate muscle tone and any involuntary movements.
Check for asymmetry in muscle contractions.
Assess cranial nerve function, particularly looking for oculogyric crises (upward deviation of the eyes) and oromandibular dystonia (jaw spasms). Systemic Examination:
Look for signs of autonomic dysfunction (e.g., sweating, tachycardia).
Assess for any signs of infection or other systemic illness that could contribute to symptoms.
Investigations
Most cases of acute dystonia are clinically diagnosed, but some investigations can help rule out other conditions or confirm the diagnosis:
Basic Blood Tests:
Full blood count (FBC) to check for infection or underlying hematological issues.
Electrolytes, including calcium and magnesium, as electrolyte imbalances can contribute to dystonia. Drug Levels:
If available and appropriate, check serum levels of suspected medications (e.g., antipsychotics) to assess for toxicity. Imaging:
Imaging is usually not required unless you suspect a structural lesion or other neurological pathology. Consider a CT or MRI brain if the presentation is atypical or if there are focal neurological signs.
Management Plan
Immediate Management:
Discontinue the offending agent: If a drug-induced cause is identified, stop the causative medication immediately.
Anticholinergic Agents: Administer anticholinergic medication such as benztropine (1-2 mg IV or IM), diphenhydramine (25-50 mg IV or IM), or procyclidine (5-10 mg IV or IM). These are first-line treatments and usually provide rapid relief.
Benzodiazepines: Consider using lorazepam (1-2 mg IV) if the response to anticholinergics is inadequate or if there is significant anxiety or agitation. Supportive Care:
Provide reassurance to the patient and their family.
Monitor vital signs, particularly if the patient is distressed or if there are signs of autonomic instability. Observation and Follow-Up:
Observe the patient until symptoms resolve, typically within an hour of treatment.
Arrange follow-up with the patient’s primary care physician or psychiatrist to review medication regimens and prevent recurrence.
Education and Prevention
Patient Education:
Educate the patient about the potential side effects of their medications and the importance of adherence to prescribed doses. Provider Education:
Ensure all healthcare providers involved in the patient’s care are aware of the reaction and the implicated medication to prevent re-prescription.
Acute dystonic reactions are an important and treatable cause of distress in the ED. A thorough history and examination, combined with prompt treatment, can rapidly alleviate symptoms and prevent recurrence. Remember to educate both the patient and the healthcare team to ensure comprehensive care.
By following these steps, junior doctors can confidently manage acute dystonic reactions, ensuring quick and effective relief for their patients.
_edited.jpg)


Comments